The Role of Neuroinflammation in Epilepsy: Unraveling the Complex Connection
Epilepsy is a neurological disorder characterized by recurrent seizures, affecting millions of people worldwide. While the exact causes of epilepsy are still not fully understood, emerging research suggests that neuroinflammation, an inflammatory response in the brain, plays a significant role in the development and progression of epilepsy. In this article, we will explore the complex connection between neuroinflammation and epilepsy, shedding light on the underlying mechanisms and potential therapeutic implications.
Understanding Neuroinflammation: The Inflammatory Response in the Brain
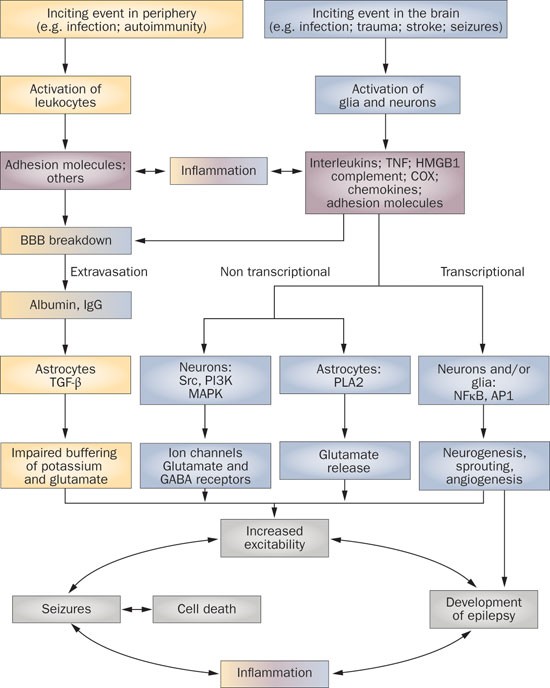
Neuroinflammation refers to the activation of the immune system in the brain, involving various immune cells, cytokines, and other inflammatory mediators. While inflammation is a natural defense mechanism against infections and injuries, chronic or excessive neuroinflammation can have detrimental effects on brain function and contribute to the development of neurological disorders, including epilepsy.
Neuroinflammation and Seizure Generation:
1. Activation of Immune Cells: During seizures, there is an activation of immune cells, such as microglia and astrocytes, in the brain. These cells release pro-inflammatory cytokines and other molecules that can disrupt the delicate balance of neuronal activity, leading to hyperexcitability and seizure generation.
2. Blood-Brain Barrier Dysfunction: Neuroinflammation can compromise the integrity of the blood-brain barrier (BBB), a protective barrier that regulates the passage of substances between the bloodstream and the brain. BBB dysfunction allows immune cells and inflammatory molecules to enter the brain, further exacerbating neuroinflammation and promoting seizure activity.
Neuroinflammation and Epileptogenesis: The Process of Epilepsy Development
1. Altered Excitatory-Inhibitory Balance: Neuroinflammation can disrupt the balance between excitatory and inhibitory neurotransmission in the brain. This imbalance, characterized by increased excitatory activity and decreased inhibitory control, creates a favorable environment for the development of epilepsy.
2. Neuronal Damage and Remodeling: Prolonged neuroinflammation can lead to neuronal damage and remodeling, including the loss of inhibitory interneurons and the formation of abnormal neuronal connections. These structural changes contribute to the generation and propagation of seizures, promoting the transition from a single seizure event to a chronic epileptic condition.
Therapeutic Implications:
1. Anti-Inflammatory Strategies: Targeting neuroinflammation holds promise as a therapeutic approach for epilepsy. Anti-inflammatory drugs, such as nonsteroidal anti-inflammatory drugs (NSAIDs) and corticosteroids, may help reduce neuroinflammation and dampen seizure activity. However, further research is needed to determine their efficacy and safety in different epilepsy subtypes.
2. Immune Modulation: Modulating the immune response in the brain may offer potential therapeutic benefits. Immunomodulatory drugs, such as minocycline and rapamycin, have shown promise in preclinical studies by reducing neuroinflammation and improving seizure control. Clinical trials are underway to evaluate their effectiveness in human epilepsy.
3. Neuroprotective Strategies: Protecting neurons from inflammation-induced damage is another avenue of research. Neuroprotective agents, such as antioxidants and antiapoptotic drugs, aim to preserve neuronal integrity and function, potentially preventing the development of epilepsy or slowing its progression.
Conclusion:
The role of neuroinflammation in epilepsy is a complex and evolving area of research. The activation of immune cells, disruption of the blood-brain barrier, altered excitatory-inhibitory balance, and neuronal damage collectively contribute to the development and progression of epilepsy. Understanding the mechanisms underlying neuroinflammation in epilepsy opens up new avenues for therapeutic interventions aimed at reducing inflammation, modulating the immune response, and protecting neurons. As research continues to advance, targeting neuroinflammation may hold the key to improving seizure control and enhancing the quality of life for individuals living with epilepsy.